ERCP (endoscopic retrograde cholangiopancreatography)
An ERCP (endoscopic retrograde cholangiopancreatography) combines an
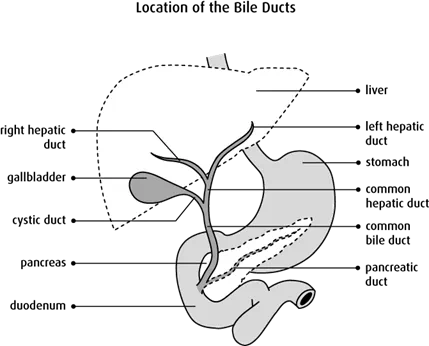
Bile is a yellowish green fluid made in the liver. It passes through the ducts from the liver, is stored in the gallbladder and then passes into a part of the small intestine called the duodenum.
Pancreatic juice is made in the pancreas. It passes through the pancreatic duct, which joins the bile duct and opens into the duodenum. Enzymes in the pancreatic juice help digest fat, carbohydrates and protein in food.
Why an ERCP is done
An ERCP is mainly done to treat a block in a bile or pancreatic duct and to collect samples of cells or tissue. A duct may become blocked by cancer or from non-cancerous causes such as stones (hard deposits) in the duct.
Because an ERCP has a higher rate of serious complications than other endoscopy procedures, it is mainly used for treatment when the bile duct is blocked. It is used less often to make a diagnosis or to check for a problem in the ducts.
Imaging tests that are less invasive and safer than an ERCP are usually used instead to examine the bile and pancreatic ducts as well as the liver, gallbladder and pancreas. These less invasive tests include a CT scan, an endoscopic ultrasonography (EUS) and a magnetic resonance cholangiopancreatography (MRCP).
An ERCP may be used for the following:
Stone removal
An ERCP is most commonly used to remove gallstones in the bile duct (also called bilestones). It is also used to remove stones in the pancreatic duct.
Sphincterotomy
A sphincterotomy is a surgery to widen or open a sphincter. The sphincter of Oddi is a muscular valve around the opening of the bile and pancreatic ducts. It controls the flow of bile and pancreatic juices into the duodenum. During a sphincterotomy, a small cut is made in the muscle. It may be used when the sphincter is narrowed (papillary stenosis) or is not working properly (sphincter of Oddi dysfunction).
Stent placement
Stents are plastic or metal devices used to widen a blocked or narrowed passage. A duct may become narrow or blocked due to scar tissue or a tumour. Stents may also be used to treat bile or pancreatic juice leaks.
A pancreatic duct stent may be used to prevent inflammation of the pancreas after an ERCP (also called post-ERCP pancreatitis).
Dilatation
If a part of the duct is narrow, it may be widened, or dilated, using a catheter (a flexible tube) with a balloon and an ERCP. A temporary stent may be placed for a few months. This is usually used to treat narrow ducts from non-cancerous causes. It may also be used to widen the sphincter of Oddi.
Diagnosis
An ERCP may be used to look for the cause of pancreatitis. An ERCP may be used to take a sample of cells with a brush or a biopsy to check for cancer cells. It is also used to measure the pressure in the pancreatic duct. The pressure may be increased if the sphincter is not working properly. An ERCP may also be used to examine the bile or pancreatic duct with an ultrasound.
Drain fluid
An ERCP may be used to drain fluid collected in the pancreas.
How an ERCP is done
An ERCP is usually done in the x-ray department of a hospital as an outpatient (you will not stay overnight). An ERCP usually takes 30–60 minutes, then you’ll stay 1–2 hours in the recovery room. Sometimes you may be in the hospital all day.
Preparation for an ERCP
Usually you will be asked not to eat or drink for 8 hours and to empty the bladder before the ERCP. You will be asked to remove clothing, jewellery, glasses and any other objects that may be in the x-ray field and may interfere with the quality of the x-ray.
During the ERCP
An anesthetic may be given to numb the throat and make it easier to put in the endoscope. You will usually be given a drug to make you relax or make you drowsy during an ERCP.
The endoscope is guided into your mouth and passed down the throat into the duodenum. You may be asked to swallow to help move the endoscope along. You may feel some discomfort. The doctor identifies the openings where the bile and pancreatic ducts drain into the duodenum (ampulla).
A small amount of air is injected through the endoscope. This makes it easier for the doctor to see the ducts. A small tube is passed through the endoscope to inject a
Special instruments may be passed through the endoscope during an ERCP:
- A small brush or forceps may be used to remove cells or a tissue sample.
- A snare or cage may be used to remove bile duct gallstones or pancreatic duct stones.
- A stent may be inserted to hold open a narrowed bile or pancreatic duct.
- A catheter with a balloon is passed through to widen a narrow duct.
When the procedure is finished, the endoscope is slowly removed. You may gag, feel nauseous or have bloating or mild abdominal cramping.
After the ERCP
After the ERCP you will be given information including:
- Do not eat or drink until the throat is no longer numb and you can safely swallow without choking.
- Do not drive for 24 hours.
- Do not return to work for 24 hours.
- You may have gas and feel bloated.
- You may have a mild sore throat, hoarseness or throat irritation.
- If gallstones are removed or a stent is inserted, you may have to stay in the hospital overnight.
Side effects
Side effects of having an ERCP may include:
- post-ERCP pancreatitis
- bleeding (hemorrhage)
- infection
- heart or lung problems
- allergic reaction to the anesthetic, dye or drug used during the procedure – can cause blurred vision, breathing problems, dry mouth, feeling hot or your face getting flushed, hives, low blood pressure, nausea, throat spasm or urine retention
- perforation of the esophagus, stomach, duodenum, bile duct or pancreatic duct – may require surgery to repair
Special considerations for children
In rare cases, child may need to have an ERCP to treat pancreatitis that comes back (recurs) or bile stones. The test is done in an operating room while the child is under a general anesthetic.
Preparing children before a test or procedure can lower anxiety, increase cooperation and help them develop coping skills. Preparation includes explaining what will happen during the test, including what they will see, feel, hear, taste or smell.
The preparation for an ERCP depends on the age and experience of the child. Find out more about helping children cope with tests and treatment.
