Colostomy and ileostomy
A colostomy creates an opening from the
A colostomy or an ileostomy can be temporary or permanent. The doctor may do a temporary colostomy or ileostomy to allow the intestine to rest and heal after surgery. It will be permanent if the anal sphincter and the lower part of the rectum are removed.
A colostomy or an ileostomy may also be called a bowel diversion.
Why a colostomy or an ileostomy is done
A colostomy or an ileostomy is done when part of the intestine needs to be removed or bypassed. A colostomy or an ileostomy may be done as part of treatment for:
- cancer of the colon, rectum or anus
- an inflammatory bowel disease, such as ulcerative colitis or Crohn’s disease
-
familial adenomatous polyposis (FAP) - a blockage in the intestine (called a bowel obstruction)
- an injury that damages the intestine
-
diverticulitis - birth defects of the intestines
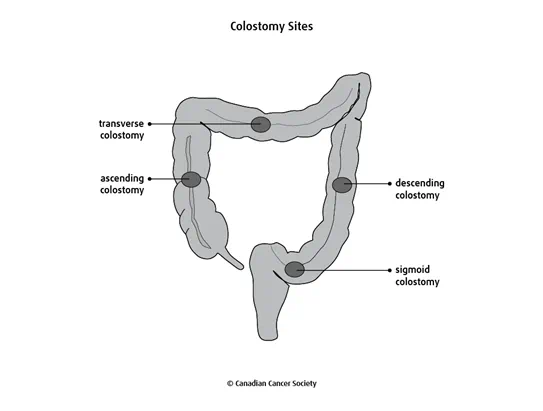
Sites of a colostomy or an ileostomy
The site of a colostomy or an ileostomy depends on the part of the intestine that is affected. The different types of colostomies are named based on where they are in the colon.
- A sigmoid colostomy is in the sigmoid colon, which is the part of the colon that connects to the rectum. A sigmoid colostomy is the most common type of colostomy.
- A descending colostomy is in the descending colon, which is the part of the colon that goes down the left side of the abdomen.
- A transverse colostomy is in the transverse colon, which is the part of the colon that goes across the upper abdomen.
-
An ascending colostomy is in the ascending colon, which is the first
part of the colon. It starts at the
cecum and goes up the right side of the abdomen. An ascending colostomy is not commonly done because doctors prefer to do an ileostomy. - An ileostomy is in the ileum, which is the last part of the small intestine.
The location of the colostomy or ileostomy will affect the type and consistency of stool (poop). Your colon normally absorbs water so when some or all of the colon is removed or bypassed, water may not be absorbed from stool as usual. For example, the stool from an ileostomy is mostly liquid because it doesn’t travel through the colon, which would normally remove most of the water. If you have a descending or sigmoid colostomy, your stool will be formed and solid as usual.
Types of colostomy and ileostomy
A colostomy or an ileostomy can be done in different ways depending on why it is needed. Your doctor will decide which type of colostomy or ileostomy is best for you.
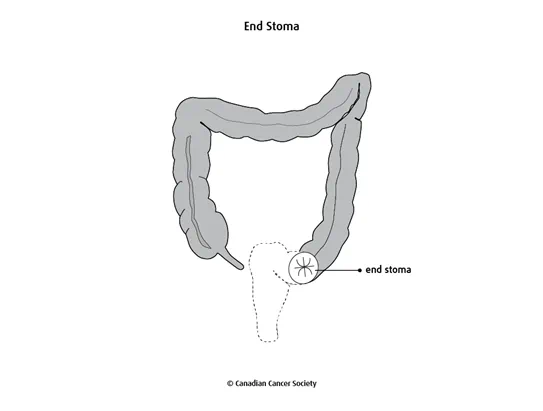
End colostomy or ileostomy
An end colostomy or ileostomy attaches one end of the colon or ileum to an opening in the abdominal wall (called the end stoma). An end colostomy is often in the sigmoid colon. An end ileostomy is often in the last part of the ileum. The rest of the colon may be completely removed.
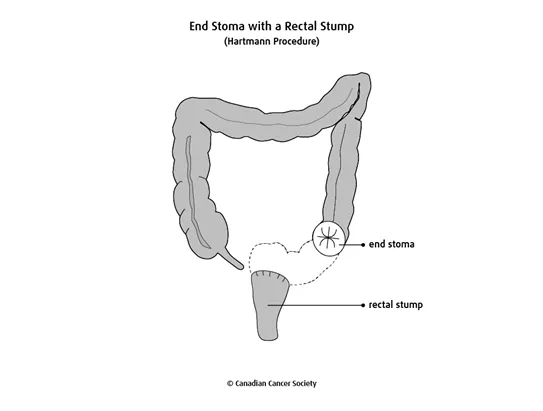
End colostomy or ileostomy with rectal stump
An end colostomy or ileostomy can be made with a rectal stump. This surgery may also be called the Hartmann procedure.
It involves attaching one end of the colon or ileum to an opening in the abdominal wall (called the end stoma). The rectum and anus are left in place, and the cut end is closed with staples or stitches. The rectal stump is not functional (stool doesn’t pass through it), but it may still make mucus that passes out of the body through the anus.
This type of colostomy or ileostomy can be temporary. After the intestine has healed, the doctor can join the remaining intestine to the rectum.
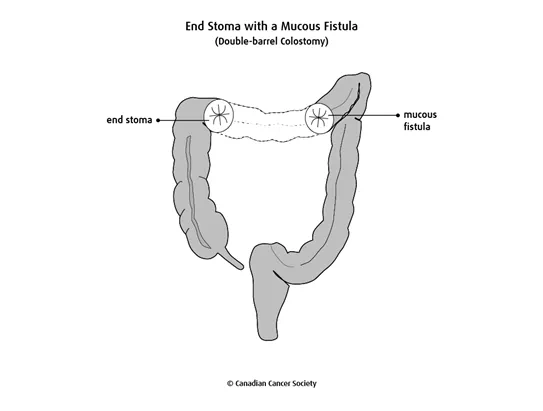
End colostomy with mucous fistula
An end colostomy with mucous fistula is also called a double-barrel colostomy. It is usually done when part of the transverse colon or descending colon is removed and the sigmoid colon, rectum and anus are not removed.
This type of colostomy is created with 2 stomas. Part of the colon is removed, and each cut end of the colon is attached to a separate opening in the abdominal wall (called the end stoma). One stoma is created from the first part of the colon on the right side of the body. This is called a functional stoma (end stoma) because stool passes through it. A second stoma (called a mucous fistula) is created from the last part of the colon. The mucous fistula passes mucus out of the body.
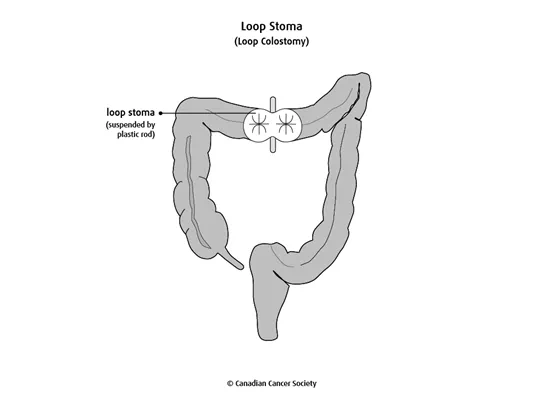
Loop colostomy or ileostomy
A loop colostomy or ileostomy is usually temporary. It is done so that stool leaves the body before it reaches the diseased or injured part of the intestine. The intestine can be connected again after it has healed.
To create a loop colostomy or ileostomy, a loop of the colon or ileum is brought out through a cut (incision) in the abdomen. A plastic rod is sometimes placed through the loop to hold it in place and to support the area during healing. Sometimes flaps of skin are used instead of a plastic rod.
The doctor then makes a cut in the colon or ileum to open it, but doesn’t cut all the way through it. The 2 sides of the opening become a stoma on the abdomen. Stool and mucus leave the body through the stoma. Some stool and mucus may also leave through the anus.
Preparing for a colostomy or an ileostomy
Before surgery, tests will be done to check your general health. Blood tests, a chest x-ray and an electrocardiogram (ECG) may be done to check the health of certain organs. Find out more about these tests and procedures.
Your healthcare team will tell you if you need to follow a special diet before surgery. They will also tell you when to stop eating and drinking before surgery.
You may need to empty your intestine before surgery. This usually means taking a laxative 1 to 2 days before surgery. You may also be given cleansing enemas at the hospital.
Your surgeon or ostomy nurse will usually mark the abdomen where the stoma will be to make sure it is in a convenient and comfortable place. Your surgeon or healthcare team may also discuss the type of pouch that you will need to use after the surgery. You may be given antibiotics before surgery to help prevent infection.
How a colostomy or an ileostomy is done
A colostomy or an ileostomy is done in a hospital using general anesthesia( you will be asleep).
The surgeon can use an open technique or a laparoscopic technique.
- With the open technique, a cut is made in the abdomen to reach the intestine.
- With the laparoscopic technique, small cuts are made in the abdomen. An endoscope and tools are inserted through the cuts to do the surgery.
The open technique is used more commonly than the laparoscopic technique for colostomy or ileostomy.
Depending on the reason for doing the colostomy or ileostomy, a bowel resection may be done first. A bowel resection is used to completely remove the diseased or damaged part of the intestine. Find out more about bowel resection.
To create an end colostomy or ileostomy, one end of the colon or ileum is brought to an opening on the surface of the abdomen. The surgeon stitches the edges of the cut part of the colon or ileum to the skin of the abdomen to make the stoma. The surgeon closes the other cut end of the colon or ileum with stitches or staples.
- For an end colostomy or ileostomy with mucous fistula, the other cut end of the colon or ileum is attached to another part of the abdomen to make a second stoma.
- For a loop colostomy or ileostomy, the surgeon stitches the cut edges of the colon or ileum to the skin on the abdomen to make a stoma with 2 openings.
A tube may be placed in the abdomen to drain fluids. This helps prevent infection and allow the area to heal properly. A special pouch (called an ostomy appliance) is placed around the stoma. This pouch collects stool that passes out of the body through the stoma.
Side effects
Side effects can happen with any type of surgery, but everyone’s experience is different. Some people have many side effects. Other people have few or none at all.
Side effects of a colostomy or ileostomy include:
- pain
- bleeding
- infection
- blood clots
- a hernia near the stoma
- the stoma falling into the abdomen
- the intestine coming out of the stoma more than expected (called prolapse)
- damage to nearby organs
- dehydration
- a bowel obstruction
Find out more about side effects of surgery.
After surgery
After surgery, you will need to stay in the hospital for several days. You will be given pain medicines to keep you comfortable. You will drink clear fluids for 1 to 2 days after surgery. Solid foods will be introduced slowly.
The stoma is usually swollen right after surgery. It is soft, moist and reddish-pink in colour, much like the lining in the mouth. There is no feeling in the stoma so it will not hurt if you touch it. There are many blood vessels on the surface of the stoma, so it may bleed a little if you rub or wipe it too hard.
When you have a colostomy or an ileostomy, you can’t control your bowel movements. You will need to wear a pouch over the ostomy all the time.
While you are in the hospital, an ostomy nurse will teach you how to live with and care for the ostomy. Before you go home, the healthcare team or ostomy nurse will talk to you about:
- changing the bandages or dressing
- showering and bathing
- how and when to take any medicines
- eating and drinking
- physical activity
- what to do if you have problems
- when to visit the surgeon for follow-up
You may be referred to an
If the colostomy or ileostomy is temporary, your healthcare team will talk to you about how long you need to have it. A temporary colostomy or ileostomy is usually in place for a few months. Once the rest of the large intestine has healed, you will have another surgery to rejoin the 2 ends of the ileum or colon. This procedure is called anastomosis. The surgeon will also close the opening on your abdomen. After this second surgery, you will be able to pass stool from the anus normally.
Managing your diet
Most people with a colostomy or an ileostomy can eat as they did before surgery. You may need to make some changes to your diet to help you manage the following problems.
Gas
Gas can be caused by certain foods and drinks. It can be difficult to control and is sometimes embarrassing. You can help control gas by eating regular meals and chewing your food slowly. You may also want to limit foods that can cause gas, including dried beans and peas, broccoli, cabbage, onions, strong cheeses and carbonated drinks.
Odour
Certain foods can cause odour from the pouch or ostomy appliance. You may want to limit foods that can cause odour, including onions, cabbage, garlic, fish, eggs and fried foods.
Some foods, including yogurt, buttermilk and parsley, can help control odour. You can also add deodorants to the pouch to control odour.
Talk to your wound, ostomy and continence (WOC) nurse if you are concerned about odour from the pouch.
Blocked or irritated stoma
Sometimes the colon or ileum can become narrow near the stoma. Certain foods may get stuck in the narrowed part of the colon or ileum and cause an obstruction (blockage). These same foods could also make the stoma swollen and irritated. An obstruction is more likely to happen with an ileostomy than with a colostomy.
Drinking extra fluids can help prevent an obstruction. You may also want to limit foods that tend to block or irritate the stoma, including nuts, popcorn, coconut, corn, celery, apples with the skin and foods with seeds, such as raspberries, strawberries and tomatoes.
Tell your doctor or healthcare team right away if you vomit or feel nauseous and nothing is coming from the stoma. You may have a blockage.
Caring for an ostomy
Specially trained nurses will teach you and your family how to care for and live with your ostomy. These nurses are called wound, ostomy and continence (WOC) nurses. They may be part of an association called Nurses Specialized in Wound Ostomy and Continence Canada (NSWOCC).
Pouch systems
If you have a colostomy, ileostomy or urostomy, a pouching system is used to collect stool or urine from the stoma. The system may have 1 or 2 pieces. They can also be closed-end or drainable.
Pouches are odour-proof even if they are full of urine or stool. There are many different pouch options to try. The pouch can’t be seen under your clothing.
A WOC nurse will help you find the system that suits your needs. They will teach you how and when to empty or change the pouch, depending on the type of stoma you have and your stool or urine output. On average, drainable pouching systems are changed twice a week. Closed-end systems are usually changed daily. It is important to change pouching systems before they leak. Don’t use tape to patch a leak because it can lead to skin problems around the stoma.
Stoma care
Your WOC nurse will teach you about cleaning the stoma and the skin around the stoma. Use only warm water and a soft cloth to clean the skin and stoma. Don’t use soap, alcohol or baby wipes because they can irritate the skin.
Showering or bathing
Your WOC nurse will teach you about showering and bathing with a stoma.
If you have a colostomy, ileostomy or urostomy, you can shower or take a bath with the pouching system on or off. The water from the bath or shower will not loosen the pouching system. The pouching system will not fall off if it gets wet. You don’t need to cover the pouching system in plastic to protect it from the water. If you have a tracheostomy, you can bathe or shower as long as the stoma is covered.
Adjusting to daily life
Talk to your WOC nurse or healthcare team about questions and concerns you have about returning to your daily life after ostomy surgery. They can help you adjust and manage your stoma during your usual activities.
Clothing
Pouching systems are designed to lie flat against your body, so you should be able to wear the same clothing you did before surgery. You can also choose to buy clothes that are specially designed for an ostomy, including underwear and swimsuits.
Physical activity
An ostomy doesn’t get in the way of most physical activities. Don’t do heavy lifting for 3 months after your surgery to allow your abdominal muscles and incision (surgical cut) to heal. A physiotherapist can help you safely strengthen your abdominal muscles. They can also help you return to your usual activities over time.
Work
You can go back to work once you recover from ostomy surgery. Some people with an ostomy may not be able to do jobs that require heavy lifting. Talk to your WOC nurse or healthcare team if you have questions or concerns about returning to work after surgery.
Travel
You can travel as you usually would after you have ostomy surgery. Travelling by airplane doesn’t affect the pouch because the cabins are pressurized. It is a good idea to travel with about twice as many supplies as you would normally use at home. Carry the supplies with you – don’t check them in with your luggage. You may also want to know where to contact a local WOC nurse during your travels.
Sex and intimacy
You can have strong, supportive relationships and a satisfying sex life after ostomy surgery. Talk to your WOC nurse, a counsellor or other people who have an ostomy if you or your partner have questions or concerns about sex and intimacy.
To find out more about intimacy after ostomy surgery, see the information published by the Ostomy Canada Society.
Emotional and mental adjustment
People who have ostomy surgery cope with both physical and psychological changes. They need to adjust to changes in their bladder and bowel function or breathing and speaking.
You may have a pouch to collect urine or stool on your abdomen or a visible trach tube. Body functions are usually private topics, so you might not feel comfortable talking about them openly. This can make you feel like you are the only one with an ostomy. But many people in Canada are living with an ostomy. Doctors, hairdressers, teachers, police officers and other people in your community may have an ostomy and you would not know.
Talk to your WOC nurse to find out more about resources in your community that can help you adjust to the emotional and mental changes that come with an ostomy. They can also tell you about support groups with trained volunteers who have been through what you are going through.
Special considerations for children
Preparing children before a test or procedure can help lower their anxiety, increase their cooperation and develop their coping skills. This includes explaining to children what will happen during the test, such as what they will see, feel and hear.
Preparing a child for a colostomy or an ileostomy depends on the age and experience of the child. Find out more about helping your child cope with tests and treatments.
Your trusted source for accurate cancer information
With support from readers like you, we can continue to provide the highest quality cancer information for over 100 types of cancer.
We’re here to ensure easy access to accurate cancer information for you and the millions of people who visit this website every year. But we can’t do it alone.
Every donation helps fund reliable cancer information, compassionate support services and the most promising research. Please give today because every contribution counts. Thank you.
