External radiation therapy
External radiation therapy is also called external beam radiation therapy. It is the most common type of radiation therapy used to treat cancer. A machine directs a beam of radiation through the skin to a specific part of the body, usually a tumour.
You can’t see or feel external radiation therapy. It doesn’t hurt and you are not radioactive after having received it. The length of a treatment session can vary depending on the type of machine used. Usually a treatment session will last about 30 minutes or longer because it takes time to set up the equipment and get you into the correct position on the table. It usually takes only a few minutes to give the dose of radiation but may be longer, depending on the type of machine being used.
External radiation therapy may be given along with chemotherapy (called chemoradiation).
External radiation therapy machines
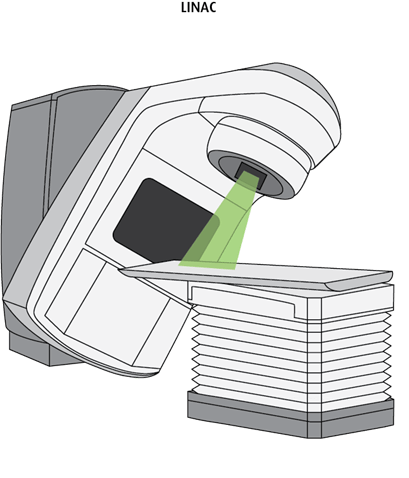
Linear accelerator (LINAC) is the most commonly used machine for giving external radiation therapy. It delivers high-energy x-rays to a particular part of the body. It can be used to treat any part of the body. Treatment is usually given over several sessions. Each session may take 15 to 30 minutes or sometimes longer.
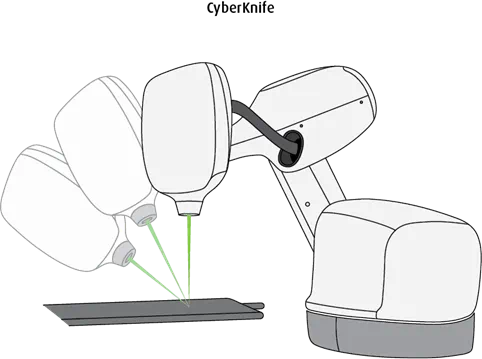
CyberKnife is a small compact linear accelerator mounted on a robotic arm that moves around the person to give radiation from many different directions. It also has several x-ray cameras (imaging devices). Computers track a person’s position and movement. If a person moves slightly, the robotic system can adjust by repositioning the linear accelerator before the beam of radiation is delivered. CyberKnife is particularly useful for treating tumours of the lung because of movement during breathing. It is most used for treating tumours of the brain, lung, prostate and spine. CyberKnife uses larger doses of radiation for each treatment than a LINAC so fewer treatment sessions are needed. Each session may take 30 to 90 minutes. Not every cancer treatment centre has a CyberKnife.
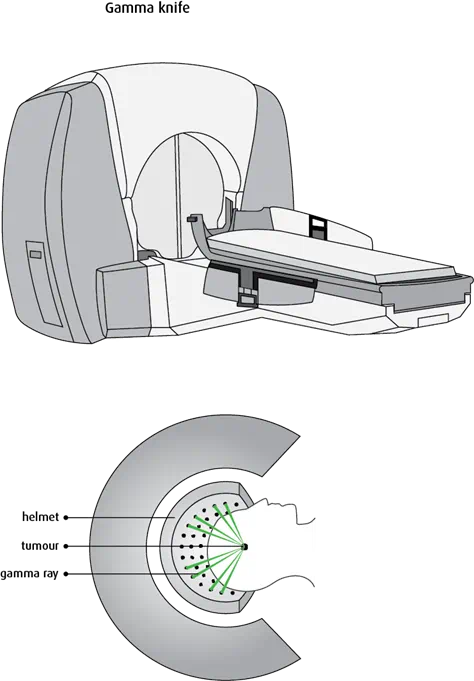
Gamma Knife is designed to give external radiation therapy to the brain. It delivers about 200 thin beams of high-energy radiation at a tumour. The highest dose of radiation is delivered at the point where the beams cross (intersect). It is usually given in a single session and used to treat primary brain tumours or brain metastases. The technique is sometimes called Gamma Knife radiosurgery.
Types of external radiation therapy
There are different techniques used when giving external radiation therapy. Some of these techniques can also be used together to deliver very precise radiation therapy.
Standard external radiation therapy uses a linear accelerator to give radiation beams to a certain area of the body. It is often given in low daily doses over a period of weeks.
3-dimensional conformal radiation therapy (3D-CRT) is a special way of giving radiation therapy that shapes the radiation beam to the tumour or treatment area. 3D-CRT uses CT or MRI images to create a precise 3D image of the tumour. The exact location and shape of the tumour is programmed into a computer and used to plan treatment. A linear accelerator is used to produce the radiation beams. Several radiation beams are then shaped and aimed at the tumour from different directions to treat the tumour from all angles. The radiation beams are all the same strength. Each individual beam is fairly weak and less likely to damage normal tissues. A higher dose of radiation is delivered where the beams cross at the tumour. 3D-CRT can be used to treat many different types of cancers.
Intensity-modulated radiation therapy (IMRT) is an advanced way of giving radiation therapy that shapes the radiation beams giving different doses to different parts of the treatment area. CT or MRI imaging is used to create a precise 3D image of the tumour. The exact location and shape is programmed into a computer and used to plan treatment. A linear accelerator is used to produce the radiation beams. Several radiation beams are then shaped and aimed at the tumour from different directions to treat the tumour from all angles. These radiation beams also vary in strength (intensity). This allows a higher dose to be delivered to the tumour and reduces the dose of radiation reaching nearby normal tissues. IMRT can be used to treat tumours that are hard to reach, such as the spine, head, neck, prostate, lung and brain.
Volumetric-modulated arc therapy (VMAT) is an advanced form of IMRT that delivers a dose to the entire tumour in a 360-degree rotation. Most modern linear accelerators can deliver this type of treatment. This shortens the daily treatment time.
Image-guided radiation therapy (IGRT) uses imaging mounted on the linear accelerator to improve the accuracy of radiation therapy. Repeated CT, MRI or PET scans are performed before and during treatment and processed by computers to show changes in tumour size and location compared to the last treatment. This allows the radiation treatment team to adjust your position on the table or the radiation dose to increase accuracy of the treatment. IGRT can lessen the amount of tissue treated and the total dose of radiation received by normal tissue. IGRT may be used to treat tumours in parts of the body that are likely to move, such as the lungs, liver and prostate, or tumours that are very close to vital structures or tissues.
Stereotactic radiosurgery (SRS) delivers precisely targeted high doses of radiation in a single session. The following types of radiation units can deliver radiosurgery: Gamma Knife, CyberKnife and linear accelerators with specific modifications. SRS creates many small, thin beams of radiation from different angles that meet at the tumour to give the highest dose to the tumour and reduce the dose of radiation to healthy tissue around the tumour. It is used most commonly to treat brain and spinal cord tumours and brain metastases. Depending on the type of machine used, you may need to wear a special head frame (stereotactic frame) during treatment. Some systems are frameless or you may only need a special mask to keep your head in position.
Stereotactic body radiation therapy (SBRT) delivers precisely targeted high doses of radiation to tumours in difficult or hard-to-reach areas in fewer sessions. It is also called stereotactic ablative radiation therapy (SABR). The majority of SBRT is delivered by modern linear accelerators but can also be delivered with a CyberKnife unit. It creates many beams of radiation from different angles that meet at the tumour. The tumour itself receives a high dose of radiation, while the individual beams that travel through surrounding tissue are a low dose. This lowers the effects of radiation on healthy tissue surrounding the tumour. SBRT is given in fewer treatments than standard external radiation therapy. It can be used to treat tumours in the pancreas, lung and liver, and tumours of the spine.
Proton therapy uses protons (positively charged particles) to treat cancer. It may also be called proton beam therapy. Proton therapy uses proton beams instead of x-ray beams. Protons release more energy after reaching a certain distance and then stop, while x-ray beams release energy before and after they hit their target. So protons cause less damage to tissues they pass through before reaching their target. Proton therapy causes the least amount of damage to nearby normal tissues. A machine called a synchrotron or cyclotron produces the protons. These machines are not available in Canada, and people may have to go to certain centres in the US to receive this treatment.
Whole brain radiation therapy (WBRT) delivers radiation therapy to the entire brain. A linear accelerator is usually used to give WBRT.
Total body irradiation (TBI) gives radiation therapy to the entire body. TBI may be used to prepare for a stem cell transplant. A linear accelerator is usually used to give TBI.
Before treatment
Your first appointment will be with the radiation oncologist. They will go over your medical records, do a physical exam and may order certain tests. They will discuss external radiation therapy, treatment options and side effects. If you have any questions about radiation therapy and your treatment, ask the radiation oncologist.
Simulation for external radiation therapy
A simulation is usually the first step in external radiation therapy. Simulation is used to help plan your radiation treatment. It is done at a cancer treatment centre, and it usually takes anywhere from 30 minutes to an hour or more. Most centres now use CT scans for simulation, and often an MRI is done if you have a brain tumour.
A machine called a simulator takes images or scans to give the healthcare team a picture of the part of the body to be treated. The most common type of simulator used is a CT (computed tomography) simulator. An x-ray simulator may also be used in some situations. A simulator is not a treatment machine. These simulations help the radiation therapy team decide where and how to direct the radiation.
You will be positioned on the simulator table, and CT images of the treatment area will be taken. The position that you should be in to receive the treatment is chosen during the simulation. You will be positioned the same way each time a treatment is given. Some things can be used to help you stay in your position.
Skin markings may be used to help position you. These act as a map and help make sure that each radiation treatment is targeted to the same area. Your skin may be marked with a pen or ink. Be careful not to wash off these temporary markings. Tiny permanent tattoos – about the size of a freckle – may also be used.
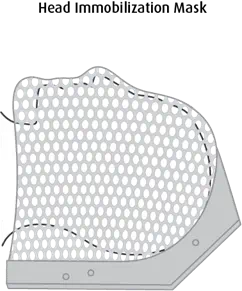
Immobilization devices may be used to help you stay in position for treatment. Forms, moulds, pads or other devices can be made from plastic, foam, plaster or other materials. Immobilization devices are specially made to fit a person’s shape. Marks to pinpoint the treatment area may be made on the mould instead of on the skin. For example, for radiation therapy to the head or neck, you may wear a mesh mask that is moulded to your face and then secured to the table to hold your head in place.
Treatment plan
After simulation, your radiation therapy team will use the information collected during simulation and enter it into a special computer program to design your treatment plan. Your treatment plan includes the total dose of radiation therapy you will receive (called the dose) and the total number of daily radiation therapy treatments.
Total dose
Total radiation dose is the total amount of radiation you will receive. It is precisely calculated and prescribed in units called grays (Gy). Depending on your treatment plan, you may receive your total dose of radiation all in one treatment or it may be divided up into several treatments over several weeks of smaller doses (called fractions). Sometimes internal radiation therapy is used along with external radiation therapy.
The total dose of radiation and the number and length of treatments depend on:
- the type of cancer
- how sensitive the tumour is to radiation therapy (radiosensitivity)
- the tumour size
- the tumour location
-
the
stage of the cancer - the amount of tissue to be radiated
- the ability of surrounding normal tissue to cope with the radiation
- whether other cancer treatments have been given or will be given
- your overall health
Many areas of the body can only cope with a certain amount of radiation in a lifetime (maximum dose). The maximum radiation dose will depend on the area of the body being treated. Doctors consider the maximum dose when planning treatment. Once an area has received the maximum dose, it may not be able to receive further radiation therapy at a later date. So having had radiation therapy in the past may limit the amount of radiation you can safely receive in the future to the same area.
Schedule
The schedule is the number of radiation therapy treatments and how often you have them. Some treatment plans last only 1 day and some may last several weeks. Usually radiation therapy is given once a day, 5 days a week, for anywhere from 1 to 8 weeks with a rest on weekends. When radiation therapy is given to relieve symptoms caused by advanced cancer (palliative radiation therapy), the course of treatment is shorter, such as a few days or 1 to 2 weeks.
Sometimes treatments are given with a different schedule, such as more than once a day or every other day.
Accelerated fractionation means giving the total dose of radiation over a shorter period of time by giving radiation more than once a day. This allows radiation treatments to be completed more quickly (for example, in 5 weeks instead of 7). Accelerated fractionation does not change the total radiation dose.
Hyperfractionation means giving the daily dose of radiation over 2 or more sessions each day. The total period of time to complete the treatment schedule is not changed. By using multiple smaller doses of radiation, a higher overall dose can be given. This may cause more damage to a cancer cell. The treatments are usually given about 4 to 6 hours apart to allow normal tissues to heal.
Hypofractionation means giving fewer larger radiation treatments over a shorter overall time. This is done by either giving a short course of larger daily treatments or giving a few large doses or a single large dose.
Radiation boost means additional radiation is given to a small area after regular radiation treatment to a larger area is finished. It is used to give additional doses of radiation to the tumour in an effort to increase the chance of controlling the tumour.
During treatment
Radiation therapy is given in the radiation therapy department of a cancer treatment centre, usually as an outpatient (you will not have to stay overnight).
Having external radiation therapy is similar to having an x-ray. Before your treatment, you may need to change into a hospital gown and remove anything metal, such as jewellery, from the treatment area.
The radiation therapist will position you on the treatment table in the same way as was done on simulation. Marks or tattoos made on the skin or alignment lasers help locate the treatment area. Immobilization devices, forms, foam wedges or rolls may be used to make sure you are in the proper position and remain still during the treatment.
If you are having stereotactic radiosurgery, you may need to have a frame placed on your head to hold it in the right position for radiation therapy. Before treatment, a neurosurgeon will attach the head frame to your skull if needed. A local anesthetic (freezing) will be used to numb the area first. Sometimes this may be done under general anesthesia for children. Depending on the type of machine used, you may use a special mask to keep your head in position.
Once you are positioned, the table will be moved under the radiation machine. The radiation therapist will measure and make sure you are in the right position. Once everything is set up properly, the therapist leaves the treatment room. The therapist controls and turns on the machine from the next room. They can see you through a window or a monitor and can talk with you through an intercom.
The radiation machine does not physically touch you. Depending on the type of machine, it moves around your body to give you radiation from different angles.
Caregivers are not allowed in the treatment room when children have treatment because they would be exposed to radiation. Depending on the treatment centre’s policy, you may be allowed to watch your child through a window into the treatment room. Or you may be asked to wait in the waiting room until the treatment is complete.
After treatment
The radiation therapy team will follow your progress throughout your treatment sessions and adjust the dose or length of treatment as needed. They may do blood tests or imaging tests at different times along your treatment to see how your tumour is responding to radiation therapy.
Recovery during and after radiation therapy will depend on the type of cancer, the stage of cancer, the radiation dose and your overall health. Some people can work and continue to do their regular leisure activities while receiving radiation therapy. Others find they tire easily and need to rest more.
The radiation therapy team will give you instructions on any limitations or special safety measures that you need to take during or after your radiation therapy. Most people are encouraged to do as much activity or exercise as they feel up to. Some people find they need extra rest for a while after treatment. Men may be told to not getting a woman pregnant during treatment and for some time after treatment, especially if radiation is given to the genital area or near it. Women may be told to not have sex if they’re having external radiation therapy to the pelvis.
Your trusted source for accurate cancer information
With support from readers like you, we can continue to provide the highest quality cancer information for over 100 types of cancer.
We’re here to ensure easy access to accurate cancer information for you and the millions of people who visit this website every year. But we can’t do it alone.
Every donation helps fund reliable cancer information, compassionate support services and the most promising research. Please give today because every contribution counts. Thank you.
