Mammography
Mammography is an x-ray of the breast that uses low doses of radiation. The picture made during mammography is called a mammogram. It can help find both cancerous (malignant) and non-cancerous (benign) tumours in the breast.
Why mammography is done
Mammography may be done for different reasons.
Screening mammography is done when there are no symptoms of breast cancer or breast problems. Both breasts are examined during a screening mammography. It can help find small lumps or abnormal areas of breast tissue before they can be felt or seen. Regular screening mammograms are important because they can monitor changes to the breast over time and find breast cancer at an early stage. Early-stage breast cancers that are small and haven't spread to other areas often have a better
Diagnostic mammography is done to diagnose a breast problem that has been found, such as a lump or nipple or skin changes. You may notice the problem and tell your doctor about it, or it may be found during a clinical breast examination or screening mammography. During a diagnostic mammography, more detailed images and views of the breast are taken from different angles, so doctors can look more closely at an area in the breast. Diagnostic mammography may be done on both breasts so that doctors can compare the breast tissue on each side.
Mammography may also be done to help find the abnormal area during a stereotactic core needle biopsy or wire localization biopsy.
Preparing for mammography
Avoid using deodorant, antiperspirant, lotions, creams, powders or perfumes under your arms or on your breasts the day of your mammography. These products can affect the accuracy of the x-ray. You may be given a disposable towel to wipe down your skin around your breasts and armpits.
It's helpful to wear a top and bra that are easy to take off. Remove necklaces and other jewellery that might get in the way during the test.
If you’re worried about discomfort during the test, these tips may help:
- Try to avoid having the test in the week before your menstrual period if your breasts are usually tender then.
- Talk to your doctor about taking a mild pain medicine about an hour before your test.
How mammography is done
Mammography is done in clinics or hospital x-ray departments.
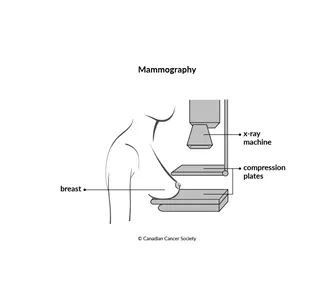
You will be asked to stand in front of the mammography machine, where your breast is placed between 2 plastic compression plates. The plates are pressed together to flatten, or compress, the breast while the radiation technologist takes an x-ray. This makes the tissues inside the breast more visible and the image in the x-ray clearer. Flattening the breast also allows less radiation to be used.
Images of each breast are taken from different angles. The compression of the breast lasts about 10 to 15 seconds per image and the entire process lasts about 20 minutes. If you have a lot of discomfort during the x-ray, tell the radiation technologist. They may be able to adjust the compression to make it more comfortable.
Before you get dressed, the technologist will check the mammography films (mammograms) to make sure they are clear enough for the radiologist (a doctor who specializes in using imaging techniques) to read. You may have to do the test again if the mammograms are not clear.
Spot compression
Spot compression (also called cone compression) may be used to get a closer view of one area of the breast during diagnostic mammography.
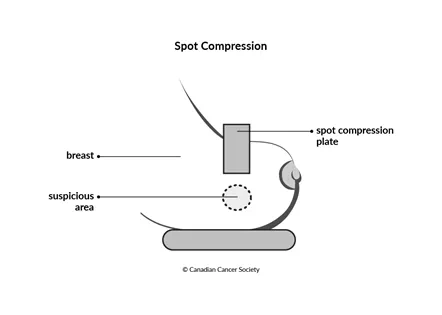
To get a clearer image, a small compression plate separates the breast tissue in an area and pushes normal breast tissue out of the way. The images may be enlarged (magnified) to make it easier to see small suspicious areas.
These close-up views can show tiny deposits of calcium (called calcifications) that look like small white spots on a mammogram. The radiologist looks at the size, shape and pattern of calcifications and includes these in the results of the mammography.
Calcifications are not breast cancer and cannot develop into breast cancer. However, they are often one of the earliest signs of breast cancer occurring in the nearby area. Calcifications can only be detected by mammography. You may need more testing if the calcifications have certain features, such as irregular shapes or groupings.
What the results mean
The radiologist will read the mammogram to look for changes or abnormalities in the breasts. Many clinics and hospitals in Canada use the American College of Radiologists Breast Imaging Reporting and Data System (BI-RADS) to report the results of the mammogram. This system recommends which follow-up tests may be needed after a mammography.
|
Your report may also say you have dense breast tissue. Dense breasts have more glandular tissue and fibrous tissue than fatty tissue. Some people have denser breasts than others. Breast density is often inherited, but other factors can affect your breast density. It is common for breasts to become less dense with age.
Having dense breasts does not mean that you will get breast cancer – but it does mean that your risk is increased.
Find out more about what it means to have dense breasts.
What happens if a change or abnormality is found
Your doctor may recommend further tests or procedures if a change or abnormality is found. Some tests or procedures that might be done include:
- diagnostic mammography, if an abnormality was found on a screening mammography
- breast ultrasound
- biopsy
- MRI
Digital mammography
Digital mammography uses an electronic image of the breast instead of x-ray film. It is sometimes called full-field digital mammography.
Digital mammography is done the same way as x-ray mammography, but the images are stored on a computer. The advantage of digital mammograms is that the images can be enlarged and changed so they can be examined in more detail. They can provide better views of suspicious or abnormal areas. Images taken during digital mammography can be sent electronically from one location to another and can be easily stored for future use or comparison.
Digital mammography may be used to further examine an abnormality found during a screening mammography or to diagnose breast cancer in hospital or clinics where this equipment is available.
Mammography with breast implants
If you have breast implants, the technologist will make sure that as much breast tissue as possible is seen on the mammogram. They will use special techniques (called implant displacement techniques) to move the implant and pull the breast tissue forward so it can be in the image. Additional images may need to be taken to examine as much of the breast tissue as possible.
The technologist will take extra care when compressing the breasts to avoid rupturing the implant.
You may be concerned about breast cancer being missed. Studies show that women with breast implants are diagnosed with breast cancer at a similar stage and have a similar prognosis as women who do not have breast implants.
Mammography safety
Modern mammography equipment uses very low doses of radiation, but having repeated x-rays does increase the risk of developing cancer. The benefits of mammography and finding breast cancer early outweigh the risk of more exposure to radiation.
Compressing the breast during mammography does not cause breast cancer. Compression does not make tumours that are already there grow or spread any faster.
Limitations of mammography
Mammography is the best test we have to find breast cancer early, but it is not perfect.
A false-negative result means that the mammogram results are normal, but there is actually cancer.
Mammography can also give a false-positive result. This means that the mammogram result suggests breast cancer when there is no cancer present. Further tests will show that many of these abnormalities are not cancer.
