Surgery for retinoblastoma
Surgery is often used to treat retinoblastoma. The type of surgery your child has depends mainly on the size of the tumour and stage of the cancer. When planning surgery, the healthcare team will also consider other factors, such as whether the retinoblastoma involves both eyes and whether vision can be saved.
Surgery may be done for different reasons. Your child may have surgery to:
- completely remove the tumour
- remove as much of the tumour as possible before other treatments, especially when vision cannot be saved
- treat retinoblastoma that comes back (recurs) or does not respond to other treatments
- reduce pain or ease symptoms (called palliative surgery)
The following types of surgery are used to treat retinoblastoma. Your child may also have other treatments before or after surgery.
Cryosurgery
Cryosurgery uses extreme cold to freeze and destroy cancer cells. During cryosurgery, the
doctor applies liquid nitrogen to the tumour of the eye through a metal tube called a
cryoprobe. This freezes the area and then scar tissue forms. The freezing may be
repeated one or more times during the same appointment. Children will be given a general
Cryosurgery may be used:
- along with chemotherapy, to treat small tumours in the eye
- if the cancer comes back after chemotherapy or radiation therapy
Find out more about cryosurgery.
Thermotherapy
Thermotherapy uses energy, such as microwaves, ultrasound or infrared radiation to deliver heat and destroy cancer cells. High temperatures can harm or kill cancer cells by damaging proteins and structures within the cells, usually with little injury to normal cells and tissues. Heat also damages tumour blood vessels so that less blood flows to the tumour.
Children will be given a general anesthetic before thermotherapy. The treatment is usually given 2 or 3 times with about one month between treatments. Each treatment lasts about 10 minutes. When thermotherapy is combined with chemotherapy, thermotherapy is usually given 1 to 2 hours after chemotherapy.
Thermotherapy may be used:
- along with chemotherapy (called chemothermotherapy or thermochemotherapy) or radiation therapy (called thermoradiotherapy) to treat small tumours in the eye
Laser surgery
Laser surgery uses a laser (a powerful beam of light) to heat and destroy cancer cells. Laser surgery is also called photocoagulation. Children are given a general anesthetic and drops to enlarge (dilate) the pupil before having laser surgery. The treatments are usually given 2 or 3 times with about one month between treatments.
Laser surgery may be used:
- to treat small tumours in the back half of the eye
- along with chemotherapy or radiation therapy
- if the cancer comes back or was not completely destroyed by chemotherapy or radiation therapy
Find out more about laser surgery.
Enucleation
Enucleation is surgery to remove the entire eyeball. This is done under a general anesthetic. There are no cuts made in the skin and no stitches. The eyelid, eye muscles, nerves and fat in the eye socket (orbit) are left in place. The surgery takes about 2 to 3 hours but your child may have to stay in the hospital for 1 to 2 days.
Enucleation is not used to treat retinoblastoma as often as it was in the past. It is now used only if other treatments are not an option. Enucleation may be used:
- to treat a large or advanced retinoblastoma
- to treat smaller retinoblastomas if other types of treatment would destroy vision or if there isn’t any useful vision in the eye
- to remove tumours that have spread throughout the eye or into the optic nerve
- if the child develops painful glaucoma (a condition of increased pressure in the eye) because of the tumour
Orbital implant
During the surgery to remove the eyeball, an eye implant (orbital implant) is usually placed in the eye socket. It is stitched into the tissues around the eye socket and onto the muscles that move the eye. These stitches do not need to be removed because they dissolve on their own. The implant is round like an eye and made of plastic, silicone or a material similar to bone. It helps fill the space where the eyeball once was and supports an artificial eye.
A temporary plastic shell with a hole in the middle (called a conformer) is often placed over the orbital implant. The conformer has an oval shape with an eye painted on it. The conformer is used while the eye area heals before an artificial eye is fitted. Some children will not have a conformer.
After surgery, the child will have a large bandage on the eye area that will stay in place for a few days to protect the eye and apply pressure to reduce swelling.
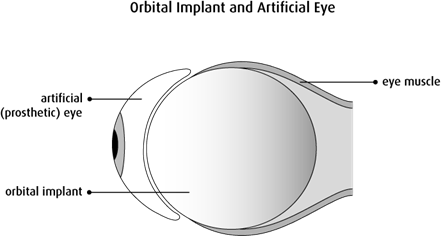
Artificial eye
Generally, the conformer is removed about 4 to 6 weeks after surgery. At this time, the child is fitted with an artificial eye (ocular prosthesis) by an ocular prosthetist or ocularist. An artificial eye is not round like an eyeball. It is a thin shell similar to a big contact lens that fits over the orbital implant and under the eyelid. The artificial eye moves in a similar way to the remaining eye, but not quite as much. The artificial eye is made to match the size and colour of the remaining eye.
Children who have an orbital implant and artificial eye are usually advised to wear glasses with shatterproof lenses to protect the remaining working eye, especially when the child plays sports. Children who wouldn’t normally wear glasses can wear ones with non-prescription lenses. Some children will need to have new implants as the bones in the face grow. A permanent implant is fitted when the child is fully grown.
Exenteration
Exenteration is surgery to remove the eyeball, eyelid, muscles, nerves and fat in the eye socket (orbit). This surgery may be used for retinoblastoma that has spread into the orbit. The orbital bone may be left in place if it doesn’t contain cancer.
The child can be fitted for an artificial eye or facial prosthesis after an exenteration. Some children will need to have new implants as the bones in the face grow. A permanent implant is fitted when the child is fully grown.
Reconstructive surgery, which may include skin and bone grafting, may be done following extensive surgery to the orbit.
In Canada, children with retinoblastoma don’t usually have exenteration because this cancer is often found before it spreads to the tissues surrounding the eye. Exenteration may be used if the cancer comes back and the child has already received the maximum acceptable doses of radiation and chemotherapy.
Side effects
Side effects can happen with any type of treatment for retinoblastoma, but every child’s experience is different. Some children have many side effects. Other children have only a few side effects.
If your child develops side effects, they can happen any time during, immediately after or a few days or weeks after surgery. Sometimes late side effects develop months or years after surgery. Most side effects will go away on their own or can be treated, but some may last a long time or become permanent.
Side effects of surgery will depend mainly on the type of surgery and your child’s overall health.
Cryosurgery, thermotherapy or laser surgery may cause these side effects:
- scarring of the eye
- damage to the retina, including retinal detachment
- swelling of the eye and eyelid
- bleeding or a blood clot
- damage to the iris
- clouding of the lens of the eye (called cataracts)
- vision problems or mild vision loss
Enucleation or exenteration may cause these side effects:
- permanent vision loss
- pain
- bleeding or a blood clot
- infection
- shifting of the orbital implant – this can be repaired with surgery to put the implant back in place
- slowed growth of the bone around the eye – this can give the eye a sunken appearance
Tell your healthcare team if your child has these side effects or others you think might be from surgery. The sooner you tell them of any problems, the sooner they can suggest ways to help your child deal with them.
Questions to ask about surgery
Find out more about surgery and side effects of surgery. To make the decisions that are right for your child, ask the healthcare team questions about surgery.
