Radiation therapy for retinoblastoma
Radiation therapy uses high-energy rays or particles to destroy cancer cells. It is sometimes used to treat retinoblastoma. The healthcare team will consider your child’s personal needs to plan the type and amount of radiation, and when and how it is given. Your child may also receive other treatments.
Radiation therapy is given for different reasons. Your child may have radiation therapy to:
- destroy the cancer cells in the body
- relieve pain or control the symptoms of advanced retinoblastoma (called palliative therapy)
The following types of radiation therapy are most commonly used to treat retinoblastoma.
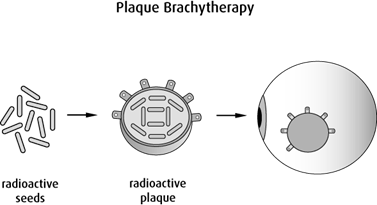
Plaque brachytherapy
Plaque brachytherapy is a type of internal radiation therapy. It may also be called surface brachytherapy. It uses a radioactive material called a radioactive isotope. Small pellets (seeds) of radioactive material are put in a container (a plaque or a disc) that is placed directly on the eyeball. The radiation kills the cancer cells over time.
The child is given a general
Some types of radioactive materials used for plaque brachytherapy include iodine-125, ruthenium-106, iridium-192 and (rarely) cobalt-60. Other radioactive materials may be used as well.
External beam radiation therapy
During external beam radiation therapy, a machine directs radiation through the eye to the tumour and some of the tissue around it.
External beam radiation therapy is not commonly used because having it at such a young age increases the risk of late effects, including the risk of second cancers in children with retinoblastoma. External beam radiation therapy may be used to treat retinoblastoma:
- with large amounts of vitreous seeding (tumours starting to form in the vitreous humour) that has not responded to other treatments like local therapies or chemotherapy
- after surgery to remove the eye, if some of the tumour is still left beyond the optic nerve
The following types of external beam radiation therapy may be used to treat retinoblastoma. They may result in fewer and less severe side effects than standard external beam radiation therapy.
Intensity-modulated radiation therapy (IMRT) is an advanced way of giving radiation therapy. It shapes the radiation beams to give different doses to different parts of the treatment area. A CT scan or an MRI is used to create a precise 3D image of the tumour.
Proton therapy uses protons to treat cancer. It may also be called proton beam therapy or conformal proton beam therapy. Proton therapy uses proton beams instead of x-ray beams. Protons only release energy after reaching a certain distance, so they cause less damage to tissues they pass through before reaching their target. Proton therapy is occasionally used for retinoblastoma. But this type of radiation therapy requires special equipment and is currently not available in Canada.
Stereotactic radiosurgery (SRS) delivers precisely targeted high doses of radiation in a single session. SRS creates many small, thin beams of radiation from different angles that meet at the tumour to give the highest dose to the tumour and reduce the dose of radiation to healthy tissue around the tumour. SRS is sometimes used to treat trilateral retinoblastoma. Trilateral retinoblastoma is when pineoblastoma develops along with retinoblastoma in both eyes (called bilateral retinoblastoma).
Side effects
Side effects can happen with any type of treatment for retinoblastoma, but every child’s experience is different. Some children have many side effects. Other children have few or none at all.
During radiation therapy, the healthcare team protects healthy cells in the treatment area as much as possible. But damage to healthy cells can happen and may cause side effects. If your child develops side effects, they can happen any time during, immediately after or a few days or weeks after radiation therapy. Sometimes late side effects develop months or years after radiation therapy. Most side effects go away on their own or can be treated, but some side effects may last a long time or become permanent.
Side effects of radiation therapy will depend mainly on the type of radiation therapy used, the size of the area being treated, the specific area or organs being treated, the total dose of radiation and the treatment schedule. Some common side effects of radiation therapy used for retinoblastoma are:
- clouding of the lens of the eye (called cataracts)
- a sunken eyeball or change in eyelid position
- inflammation of the cornea or conjunctiva
- dry eyes
- damage to the retina (called radiation retinopathy)
- bleeding from the eye
- increased pressure in the eye (called glaucoma) that can lead to blindness
- vision problems
- loss of hair in the treated area (eyelashes or eyebrows)
- fatigue
- skin problems
Other side effects can develop months or years after treatment for retinoblastoma. Find out more about late effects of treatments for retinoblastoma.
Tell your child’s healthcare team if your child has these side effects or others you think might be from radiation therapy. The sooner you tell them of any problems, the sooner they can suggest ways to help your child deal with them.
Questions to ask about radiation therapy
Find out more about radiation therapy and side effects of radiation therapy. To make the decisions that are right for your child, ask the healthcare team questions about radiation therapy.
