Whipple procedure
The Whipple procedure removes a pancreatic tumour, tissue around the tumour, and
parts of the pancreas. It also removes the
The Whipple procedure is also known as a pancreaticoduodenectomy.
Why a Whipple procedure is done
A Whipple procedure may be done to treat:
- pancreatic cancer
- bile duct cancer
- small intestine cancer
- neuroendocrine cancer
-
cancer of the
ampulla of Vater - other tumours or disorders of the pancreas, duodenum or bile ducts
How a Whipple procedure is done
The Whipple procedure is done in the hospital using general anesthesia( you will be asleep).
The surgeon makes a large cut (incision) in your abdomen. (A Whipple procedure
is sometimes done as a
The surgeon checks the organs and lymph nodes in the abdomen to make sure the cancer hasn’t spread and can be completely removed. Tissue samples are taken for biopsy.
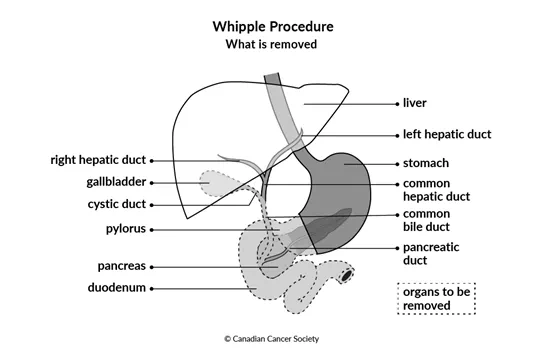
The surgeon then removes the tumour, tissue around the tumour, parts of the pancreas, the duodenum, the pylorus (lower part of the stomach), the gallbladder, part of the common bile duct and nearby lymph nodes.
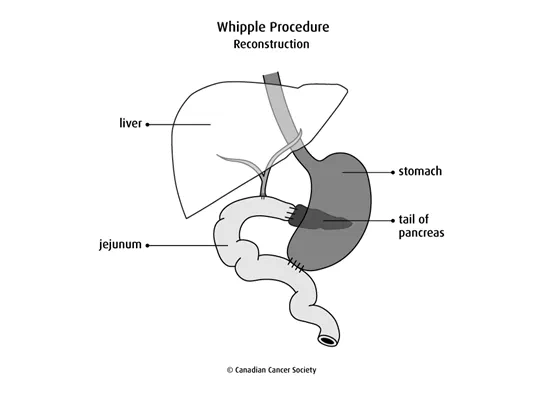
After removing these organs, the surgeon attaches the remaining end of the
stomach to the
Modified Whipple procedure
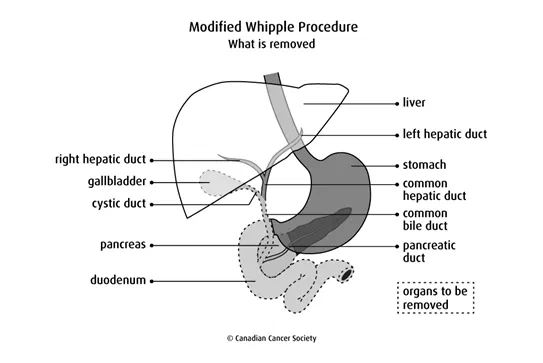
A modified Whipple procedure removes the same organs as the Whipple procedure except for the pylorus. This surgery doesn’t remove any of the stomach, so the stomach can still work normally.
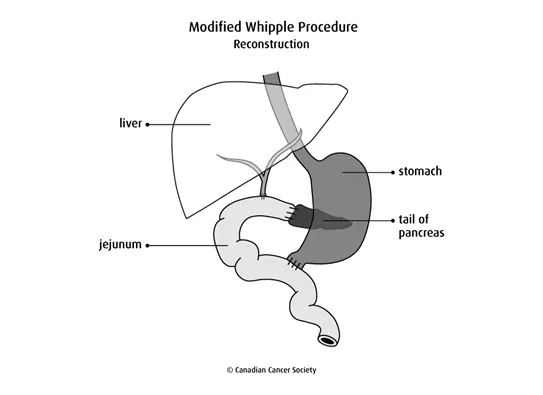
After removing these organs, the surgeon attaches the remaining duodenum (that is connected to the stomach) to the jejunum. The rest of the common bile duct and pancreas are also attached to the jejunum so that bile and pancreatic juices can flow into it.
After surgery
After surgery, you will stay in the hospital for 1 to 2 weeks.
- You will be given pain medicine to keep you comfortable.
- You will be given fluids intravenously until you can eat and drink again. You may also have a feeding tube. When you can eat and drink again, you will first be offered clear fluids. Solid foods and meals will be introduced slowly.
- You may have a catheter to drain urine (pee) from your bladder into a bag. You will also have drainage tubes to collect any extra fluid or blood. These tubes will be removed after a few days.
- After part of the pancreas is removed, the rest of the pancreas may not make enough insulin to control blood sugar. You may be given insulin injections. Injections are usually only needed until the pancreas recovers from surgery and starts to make insulin again.
- You may also need to take digestive enzymes by mouth to help your body break down and absorb fats and proteins.
Side effects
Side effects can happen any time during, immediately after or a few days or weeks after a Whipple procedure. Sometimes late side effects develop months or years after surgery. Most side effects will go away on their own or can be treated, but some may last a long time or become permanent.
The Whipple procedure carries a high risk for complications. Tell your healthcare team if you have any of the following side effects.
Pain can be caused by damage to tissue. It may take time for the pain to go away. Pain-relieving medicines can help you control the pain. Find out more about pain.
Infection can happen after surgery. Tubes may be placed around the infected wound to drain extra fluids. Your doctor may also prescribe antibiotics to help prevent or treat an infection. Find out more about infection.
Bleeding( hemorrhage) can happen if a blood vessel is not sealed off during surgery or if you have a blood clotting disorder. You may bleed a small amount after surgery.
Anastomotic leak is when bile, stomach acid or pancreatic juices leak from where the healthy ends of the stomach, duodenum or bile duct were joined to the jejunum.
Delayed gastric emptying is a condition where food stays in the stomach longer than usual. Delayed gastric emptying can cause nausea, vomiting and a full feeling. It usually goes away 4 to 12 weeks after surgery. You may need a feeding tube to make sure you get enough nutrition. Delayed gastric emptying is more common after a modified Whipple procedure than a Whipple procedure.
Dumping syndrome is when food moves too fast from the stomach into the small intestine. It may also be called rapid gastric emptying. Dumping syndrome is more common after a Whipple procedure than a modified Whipple procedure. Find out more about dumping syndrome.
Nutrition problems can happen after surgery when there is a lack of digestive enzymes, pancreatic juices or bile. This can cause poor appetite, poor fat absorption, diarrhea, bloating and indigestion. You may need to take digestive enzymes.
Your trusted source for accurate cancer information
With support from readers like you, we can continue to provide the highest quality cancer information for over 100 types of cancer.
We’re here to ensure easy access to accurate cancer information for you and the millions of people who visit this website every year. But we can’t do it alone.
Every donation helps fund reliable cancer information, compassionate support services and the most promising research. Please give today because every contribution counts. Thank you.
