Neck dissection
A neck dissection is a surgery to remove lymph nodes from the neck. The lymph nodes in the neck are called cervical lymph nodes. This surgery is also called a cervical lymph node dissection or a cervical lymphadenectomy.
The lymph nodes are part of the lymphatic system. The lymphatic system helps fight infections and is made up of lymph vessels, lymph fluid, lymph nodes, bone marrow and the lymphatic organs (thymus, adenoid, tonsil and spleen).
Lymph vessels are thin tubes similar to blood vessels. They collect and move lymph fluid away from tissues into the lymph nodes. Lymph nodes are small bean-shaped organs of lymphatic tissue. The lymph fluid can carry cancer cells from where the cancer started into the lymph nodes. With head and neck cancers, the lymph fluid can sometimes carry cancer cells into the cervical lymph nodes.
In the early stages, you usually cannot feel the cancer in the lymph nodes. In more advanced stages of cancer, you may feel a lump in the neck as the lymph nodes in the neck get bigger.
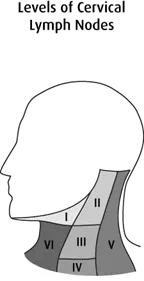
The cervical lymph nodes are grouped into different levels based on where they are in the neck.
|
Level |
Name |
Location |
|---|---|---|
|
I |
submental and submandibular nodes |
under the chin and lower jaw |
|
II |
high jugular or upper deep cervical nodes |
at the top part of the jugular vein |
|
III |
middle deep cervical nodes |
in the middle area around the jugular vein |
|
IV |
low jugular nodes |
at the lower part of the jugular vein |
|
V |
posterior jugular nodes |
around the collarbone, shoulder and back of the neck (posterior triangle) |
|
VI |
anterior (central) compartment lymph nodes |
the area in the middle of the neck, between the carotid arteries (blood vessels that carry blood to the neck, face and brain) |
Why a neck dissection is done
A neck dissection is done to:
- check for cancer in the lymph nodes in the neck
- remove lymph nodes that may contain cancer
- remove lymph nodes when there is a high chance cancer will spread to them
- reduce the chance that the cancer will come back (recur)
- remove cancer that is still in the lymph nodes after radiation therapy or chemotherapy
- help doctors plan further treatment
How a neck dissection is done
A neck dissection is done under general
You may have a neck dissection at the same time as surgery to remove the main tumour or as a separate surgery. The surgeon makes a cut (incision) in the neck to remove the lymph nodes. Depending on the type of neck dissection surgery, the surgeon may also remove other tissue in the area.
Selective neck dissection removes only those lymph nodes where cancer is very likely to spread. How many and which lymph nodes are removed is based on the size and location of the primary tumour. The muscle and nerve tissue around the lymph nodes are not removed to maintain proper function of the neck and shoulder. A selective neck dissection is also called a functional neck dissection.
Modified radical neck dissection removes lymph nodes from levels I to V, but keeps one or more of the following – internal jugular vein, sternocleidomastoid muscle or spinal accessory nerve.
Radical neck dissection removes nearly all lymph nodes on one side of the neck as well as the internal jugular vein, sternocleidomastoid muscle and spinal accessory nerve.
After removing the lymph nodes, the surgeon places a small tube (drain) in the wound and closes the cut with stitches or staples. A drainage bag is attached to the end of the tube to collect fluid draining from the area. This reduces the chance of fluid building up in the tissue and improves healing. The drain is left in place for a few days or until there is little drainage.
After a neck dissection, you may need to stay in the hospital for a few days. You may be given:
- antibiotics to prevent infection (if the primary tumour is removed at the same time)
- pain-relieving medicine
- instructions on caring for and dressing the wound
- advice on how much and which types of activity you can do after surgery
- advice on body positions that may help reduce swelling
- a follow-up appointment to see the surgeon in 1–2 weeks
- information about which symptoms and side effects you should report
The lymph nodes and any other tissue removed during surgery are sent to a lab to be examined by a doctor who specializes in the causes and nature of disease (pathologist).
Side effects
If you develop side effects, they can happen any time during, immediately after or a few days or weeks after a neck dissection. Sometimes late side effects develop months or years after a neck dissection. Most side effects will go away on their own or can be treated, but some may last a long time or become permanent.
Tell your healthcare team if you have these side effects or others you think may be from a neck dissection:
- pain and stiffness
- bruising
- signs of infection, such as pain, redness, yellow discharge (pus) or fever
- a collection of fluid under the skin (seroma) in the neck near the cut
- swelling due to a buildup of lymph fluid in the soft tissues (lymphedema)
- changes in the shape of the neck
- shoulder pain and a change in the normal shape, with some weakness on the side of the surgery
The healthcare team may give you antibiotics to prevent or treat an infection, or they may drain a buildup of fluid. Lymphedema treatment may include massage therapy and exercises.
What the results mean
Each lymph node removed is examined to see if it contains cancer.
- A negative lymph node has no cancer cells.
- A positive lymph node has cancer cells.
The pathologist’s report includes the type of cancer, the number of lymph nodes removed and the number of lymph nodes that have cancer cells. The report may also say if the cancer has grown through the outer covering of the lymph node (the capsule).
Doctors use the number of positive lymph nodes to help
Depending on the result, your doctor will decide if you need more tests, any treatment or follow-up care.
Special considerations for children
In rare cases, a neck dissection may be done in children to treat cancers that may spread to lymph nodes in the neck, such as melanoma or thyroid cancer.
Preparing children before a test or procedure can lower anxiety, increase cooperation and help them develop coping skills. Preparation includes explaining to children what will happen during the test, including what they will see, feel, hear, taste or smell.
Preparing a child for a neck dissection depends on the age and experience of the child. Find out more about helping your child cope with tests and treatment.
