Colonoscopy
A colonoscopy lets a doctor look at the lining of the entire colon and rectum using
an
A virtual colonoscopy uses a CT scan or an MRI to make an image of the lining of the colon and rectum. Researchers are still studying virtual colonoscopy to see if the results are as accurate as a regular colonoscopy. It is not offered in all clinics.
Why a colonoscopy is done
A colonoscopy may be done to:
-
look for causes of blood in the stool (poop),
anemia , abdominal pain or changes in bowel habits, such as constipation or diarrhea - look for areas of inflammation that may show ulcerative colitis or Crohn’s disease
- follow up after abnormal results from other tests, such as a stool test, a barium enema, a CT scan or an MRI
- collect tissue for testing (called a biopsy)
-
check for colorectal cancer or
polyps - follow up after surgery for colon cancer
Screening for colorectal cancer may include colonoscopy for people at high risk. Find out more about screening for colorectal cancer.
How a colonoscopy is done
A colonoscopy is done in a hospital, clinic or doctor’s office. It usually takes about 30 to 45 minutes, but it can take longer.
Preparation for a colonoscopy usually includes:
- following a liquid diet for 1 to 2 days before the test
- taking a laxative, having an enema or both to completely empty the colon
You can expect the following during a colonoscopy:
- An intravenous (IV) line may be placed in your arm so that medicines, including sedation, pain medicine and antibiotics, can be given.
- You will be asked to lie on your left side with your knees pulled up. You may be asked to change positions during the test.
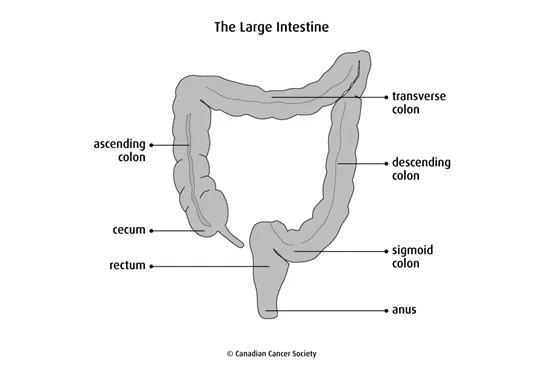
- The doctor will insert the endoscope through the anus and into the rectum and colon. The colon will be inflated with air to stretch out the lining so that the doctor can check the entire surface.
- Instruments can be passed through the endoscope to perform biopsies, remove polyps and stop bleeding.
- You may have some cramping or feel like you need to have a bowel movement while the scope is in your colon. You may feel and hear gas passing around the scope.
After the test, it is normal to have some mild abdominal cramping and passing of gas. You will be asked to stay at the clinic for 1 to 2 hours after the test.
If you were sedated during the test, you won’t be able to drive or operate machinery for 24hours. Make sure you have someone to drive you home after the test.
Ask the doctor about when you can continue your normal diet, medicines and activities.
Side effects
Common side effects of colonoscopy include:
- small amounts of blood in the stool for 1 to 2 days if a biopsy was done or if a polyp was removed
- nausea, vomiting, bloating or irritation of the rectum
Uncommon but serious side effects include:
- a small hole (puncture) in the bowel, which is treated with antibiotics and sometimes surgery to repair the hole
- heavy bleeding, which may be treated with a blood transfusion, another colonoscopy or surgery to stop the bleeding
- an allergic reaction to the medicine used for sedation
What the results mean
An abnormal result may show:
- diverticulosis (abnormal pouches in the lining of the colon)
- hemorrhoids
- inflammatory bowel disease (ulcerative colitis or Crohn’s disease)
- bleeding in the colon or rectum
- polyps
- cancer of the colon or rectum
What happens if the results are abnormal
Your doctor may recommend more tests, procedures, follow-up care or treatment.
Special considerations for children
Preparing children before a test or procedure can help lower their anxiety, increase their cooperation and develop their coping skills. This includes explaining to children what will happen during the test, such as what they will see, feel and hear.
Preparing a child for a colonoscopy depends on the age and experience of the child. Find out more about helping your child cope with tests and treatments.
Your trusted source for accurate cancer information
With support from readers like you, we can continue to provide the highest quality cancer information for over 100 types of cancer.
We’re here to ensure easy access to accurate cancer information for you and the millions of people who visit this website every year. But we can’t do it alone.
Every donation helps fund reliable cancer information, compassionate support services and the most promising research. Please give today because every contribution counts. Thank you.
