What is prostate cancer?
Check out this factsheet for a summary of the video.
Prostate cancer starts in the cells of the prostate. A cancerous (malignant) tumour consists of cancer cells that can grow into nearby tissue and destroy it. The tumour can also spread (metastasize) to other parts of the body.
Prostate cancer is the most common cancer in Canadian men. It is most common in older men. It is more common in Black men (including men of African and Caribbean ancestry) than in white men, and it is less common in Asian men. Trans women and non-binary people who were assigned male at birth can also get prostate cancer.
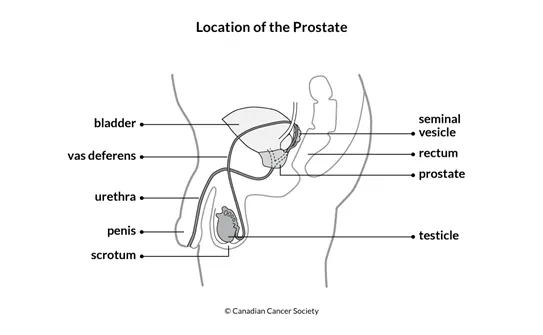
The prostate is part of the male reproductive and urinary systems. It makes some of the fluid that is part of semen. It is located below the bladder and in front of the rectum. The urethra (tube that carries urine, or pee, and semen out of the body through the penis) goes through the prostate.
The prostate is usually about the size of a walnut in younger men but can change as you age and grow larger in older men.
Prostate cancer usually grows slowly and can often be completely removed or successfully managed when it is diagnosed before it has spread outside of the prostate. Older men with prostate cancer often die of other causes. Adenocarcinoma of the prostate is the most common type of prostate cancer. It accounts for 95% of all prostate cancers.
Adenocarcinoma
Adenocarcinoma starts in gland cells. Gland cells in the prostate make mucus and prostatic fluid, which mix with sperm and other fluids to make semen. Most adenocarcinomas are found in the outer part of the prostate.
Adenocarcinoma usually develops in more than one area (site) of the prostate. When cancer is found in more than one area of an organ it is called multifocal cancer. Each site in the prostate can have a different
Rare cancerous tumours of the prostate
The following cancerous tumours of the prostate are rare:
- urothelial carcinoma (also called transitional cell carcinoma)
- sarcoma
- small cell carcinoma
- carcinoid tumours
- squamous cell carcinoma
Possible precancerous conditions of the prostate
Precancerous conditions of the prostate are changes to prostate cells that could make them more likely to develop into cancer. These conditions are not yet cancer. But if they aren't treated, there is a chance that these abnormal changes will become prostate cancer.
Some experts classify prostatic intraepithelial neoplasia (PIN), proliferative inflammatory atrophy (PIA) and atypical small acinar proliferation (ASAP) as precancerous conditions, but most experts don't think they are linked to a higher chance of developing prostate cancer. So those with PIN, PIA and ASAP aren't treated, and only those who have ASAP need follow-up.
Prostatic intraepithelial neoplasia (PIN) is an abnormal condition of the
Proliferative inflammatory atrophy (PIA) means that there are areas of inflammation in the prostate and the prostate cells look smaller than normal. PIA is not cancerous. Some research suggests a link between PIA and high-grade PIN or prostate cancer and some research does not.
Atypical small acinar proliferation (ASAP) is an abnormal growth of gland cells in the prostate. Some men with ASAP may have prostate cancer, so doctors may recommend doing a follow-up biopsy in 6 months. If the repeat biopsy also shows ASAP, doctors may recommend treatment.
Non-cancerous conditions of the prostate
A non-cancerous (benign) condition of the prostate is a change to prostate cells, but it is not cancer. Non-cancerous conditions do not spread (metastasize) to other parts of the body and are not usually life-threatening.
The most common non-cancerous conditions of the prostate are:
