Chemotherapy for childhood leukemia
Chemotherapy uses anticancer (cytotoxic) drugs to destroy cancer cells. Most children with leukemia have chemotherapy. The healthcare team will consider your child’s personal needs to plan the drugs, doses and schedules of chemotherapy. Your child may also receive other treatments.
Chemotherapy is given for different reasons. Your child may have chemotherapy to:
- destroy leukemia cells, go into remission and return blood cell production to normal
- destroy leukemia cells in the brain and spinal cord (called the central nervous system, or CNS) and prevent leukemia cells from spreading to the CNS
- prepare for a stem cell transplant
Chemotherapy is usually a systemic therapy. This means that the drugs travel through the blood to reach and destroy cancer cells all over the body. The drugs are often given through a needle in a vein (intravenously). Your child may need intense chemotherapy and a special device called a central venous catheter may be used to safely give the drugs. It is usually placed during surgery at the start of chemotherapy and left in place until treatment is finished.
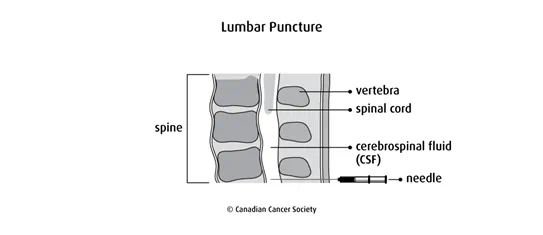
Chemotherapy may also be a regional therapy, which means that it is given to a specific area of the body. Most children with leukemia will have chemotherapy injected into the fluid around the spinal cord (called the cerebrospinal fluid, or CSF).
Intrathecal chemotherapy is given through a lumbar puncture (spinal tap) into the CSF.
Chemotherapy drugs used for childhood leukemia
Chemotherapy drugs used to treat childhood leukemia will depend on the type of leukemia – acute lymphocytic leukemia or acute myelogenous leukemia.
If childhood leukemia does not respond to drugs used in earlier treatments or if it comes back, some of the drugs used in the original treatment may be repeated. Sometimes the doses of the drugs are increased.
Side effects
Side effects can happen with any type of treatment for childhood leukemia, but every child’s experience is different. Some children have many side effects. Other children have only a few side effects.
Chemotherapy may cause side effects because it can damage healthy cells as it kills cancer cells. Side effects can happen at any time during, immediately after or a few days or weeks after chemotherapy. Sometimes late side effects develop months or years after chemotherapy. Most side effects go away on their own or can be treated, but some side effects may last a long time or become permanent.
It is hard to say exactly which side effects a child will have, how long they will last and when the child will recover. A child’s body seems to handle chemotherapy better than an adult’s body. Children usually have less severe side effects and will often recover from them faster than adults.
Side effects of chemotherapy will depend mainly on the type of drug, the dose, how it’s given and your child’s overall health. Some common side effects of chemotherapy drugs used for childhood leukemia are:
- low blood cell counts
- sore mouth and throat
- loss of appetite
- taste changes
- nausea and vomiting
- hair loss
- nervous system damage
- constipation
- weight loss
- diarrhea
- skin problems
- fatigue
- muscle and joint pain
- heart problems
- female reproductive system problems
- male reproductive system problems
Other side effects can develop months or years after treatment for childhood leukemia. Find out more about late effects for childhood leukemia.
Tell your child’s healthcare team if your child has these side effects or others you think might be from chemotherapy. The sooner you tell them of any problems, the sooner they can suggest ways to help your child deal with them.
Information about specific cancer drugs
Details on specific drugs change regularly. Find out more about sources of drug information and where to get details on specific drugs.
Questions to ask about chemotherapy
Find out more about chemotherapy and side effects of chemotherapy. To make the decisions that are right for your child, ask the healthcare team questions about chemotherapy.
