Radiation therapy for eye cancer
Radiation therapy uses high-energy rays or particles to destroy cancer cells. Most people with eye cancer will have radiation therapy. Radiation therapy can help save your vision. It is used more often than surgery to treat eye cancer. Your healthcare team will consider your personal needs to plan the type and amount of radiation, and when and how it is given. You may also receive other treatments.
Radiation therapy is given for different reasons. You may have radiation therapy to:
- destroy the cancer cells in the eye
- shrink a tumour in the eye before other treatments such as surgery
- destroy cancer cells left behind after surgery or chemotherapy to reduce the risk that the cancer will come back (recur) (called adjuvant therapy)
- relieve pain or control the symptoms of advanced eye (called palliative therapy)
The following types of radiation therapy are most commonly used to treat eye cancer.
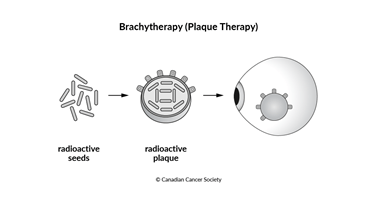
Brachytherapy
Brachytherapy is a type of radiation therapy that uses a radioactive material called a radioactive isotope. It is placed right into the tumour or very close to it. Radioactive materials can also be placed in the area from where the tumour was removed. The radioactive materials give off radiation that kills the cancer cells over time.
Brachytherapy for eye cancer is also called episcleral plaque therapy. Radioactive seeds are attached to a circular piece of metal (called a plaque). The plaque is made of gold, which helps to protect nearby tissues from radiation.
The plaque is placed over the eye tumour with surgery. A local anesthetic is used to freeze the area. The plaque is sewn into the white part of the eye (the sclera) to keep it in place. This procedure takes about 1–2 hours. The plaque is left in the eye for about 4–7 days, depending on the size of the tumour and the dose of the radiation. Surgery is used to remove the plaque.
External beam radiation therapy
During external beam radiation therapy, a machine directs radiation through the skin to the tumour and some of the tissue around it. It is most often used to treat lymphoma of the eye, but it is sometimes used to treat melanoma of the eye. Different types of external beam radiation therapy are used to treat eye cancer, including stereotactic radiation therapy and proton beam radiation therapy.
Before having external beam radiation therapy, you may need surgery to put metal clips (tags) in the back of the eye. The clips are put in under a general anesthetic (you will be unconscious) and stay in place after treatment but do not affect vision. These metal clips help to better aim the radiation at the part of the eye with the tumour.
For some types of eye cancer, such as a cancerous tumour in the eyelid, the lens of the eye is shielded to protect it during radiation therapy.
Proton beam radiation therapy
Proton beam radiation therapy is a type of charged particle radiation therapy. It uses high-energy (charged) proton particles instead of x-ray beams. Protons deliver a higher dose of radiation but cause less damage to nearby tissues than conventional external beam radiation therapy because they can be aimed more precisely at the tumour. Proton beam radiation therapy is not widely available in Canada.
Stereotactic radiation therapy
Stereotactic radiation therapy is another type of external beam radiation therapy that is used to treat melanoma of the eye. Stereotactic radiation therapy allows radiation beams to be given to a specific area. It may be used for large eye tumours or tumours close to the optic nerve when brachytherapy can’t be used.
Side effects
Side effects can happen with any type of treatment for eye cancer, but everyone’s experience is different. Some people have many side effects. Other people have few or none at all.
During radiation therapy, the healthcare team protects healthy cells in the treatment area as much as possible. But damage to healthy cells can happen and may cause side effects. If you develop side effects, they can happen any time during, immediately after or a few days or weeks after radiation therapy. Sometimes late side effects develop months or years after radiation therapy. Most side effects go away on their own or can be treated, but some side effects may last a long time or become permanent.
Side effects of radiation therapy will depend mainly on the size of the area being treated and the specific area being treated, the type of radiation therapy, the total dose of radiation and the treatment schedule. A common side effect of radiation therapy used for eye cancer is damage to the treated eye, such as:
cataracts - a tear in the retina (detached retina)
- an increase in pressure in the eye (glaucoma)
- damage to the blood vessels in the retina (radiation retinopathy)
- bleeding from the eye
Other common side effects are:
- vision changes, poor vision or loss of vision in the treated eye
- loss of eyelash or eyebrow
- a dry, red or teary eye
- sensitivity to light
- skin problems
- fatigue
- change in eyelid position
Tell your healthcare team if you have these side effects or others you think might be from radiation therapy. The sooner you tell them of any problems, the sooner they can suggest ways to help you deal with them.
Questions to ask about radiation therapy
Find out more about radiation therapy and side effects of radiation therapy. To make the decisions that are right for you, ask your healthcare team questions about radiation therapy.
