Endoscopic treatments
Endoscopic treatments are done using an endoscope (a thin, tube-like instrument with a light and lens) placed in the esophagus. You may be offered endoscopic treatments to relieve the symptoms of advanced esophageal cancer, such as difficulty swallowing. This is called palliative therapy. Some endoscopic treatments may also be used to treat precancerous conditions and early stage cancers in the esophagus.
Endoscopic mucosal resection (EMR)
EMR is an endoscopic treatment used to remove the inner layer, or mucosa, of the esophagus. The doctor passes an endoscope through the mouth, down the throat and into the esophagus. The tumour is lifted away from the wall of the esophagus using suction. A special tool is passed through the endoscope to the tumour. This tool uses an electrical current to remove the tumour along with a margin of healthy tissue around it. The electrical current stops bleeding as it cuts the tissue.
After EMR, the healthy tissue removed along with the tumour is examined under a microscope. If cancer cells are found in the tissue, more EMR or treatment with chemotherapy, radiation therapy or photodynamic therapy (PDT) may be needed to completely remove or destroy the cancer.
EMR may be used to treat small, very early stage tumours that are in the mucosa of the esophagus that haven't spread to the other layers of the esophagus. It may also be used to treat a precancerous condition called Barrett's esophagus.
Endoscopic submucosal dissection (ESD)
Endoscopic submucosal dissection (ESD) is similar to EMR. With this procedure, salt water is injected in the submucosa layer under the tumour to lift it away from the wall of the esophagus.
Radiofrequency ablation (RFA)
Radiofrequency ablation (RFA) uses a high-frequency electrical current to destroy cancer cells. The doctor places an endoscope with a balloon connected to the end into the esophagus beside the area of the esophagus that will be treated. The balloon is inflated so that the walls of the balloon touch the abnormal area. A high-frequency electrical current is given through the wall of the balloon. The balloon may be moved to treat other abnormal areas in the esophagus.
RFA may be used to treat Barrett's esophagus. It may be offered as an alternative to surgery for stage 0 esophageal cancers so that the esophagus doesn't have to be removed.
RFA may also be used to treat symptoms of advanced esophageal cancer, such as difficulty swallowing.
Laser surgery
Laser surgery uses an intense beam of light to make bloodless cuts in tissue. To treat abnormal areas in the esophagus, an endoscope with a laser attached is used to remove tissue. The type of laser used is called a neodymium: yttrium-aluminum-garnet (Nd:YAG) laser.
Laser surgery is used to relieve pain or remove a blockage caused by an esophageal tumour.
Photodynamic therapy (PDT)
Photodynamic therapy (PDT) uses a photosensitizer drug to make cells sensitive to light. The most common PDT drug used to treat esophageal cancer is porfimer (Photofrin).
PDT is given in 2 stages. First, the photosensitizing drug is injected into a vein. All cells take up (absorb) the drug from the blood, but it stays in the cancer cells longer than in normal cells.
After a certain amount of time, your doctor will expose the cancer cells to a low intensity laser light. This laser light is attached to an endoscope, which is placed through your mouth and down your throat into the esophagus. The photosensitizer in the cancer cells absorbs the light and a chemical reaction occurs that kills the cancer cells. Most normal cells are not affected.
Sometimes you may need to have a second PDT treatment so that the area is completely treated. PDT only destroys cancer cells in the inner layer, or mucosa, of the esophagus that can be reached by the light. It can't be used for large tumours or esophageal cancer that has spread into deeper layers of the esophagus or to other parts of the body. It may be offered as a treatment for Barrett's esophagus, or if you can't have other endoscopic therapies or surgery. It may also be used to remove abnormal areas in the esophagus that are left behind after EMR.
PDT may also be offered to people with advanced esophageal cancer to relieve pain or make swallowing easier.
You will need to take special precautions after PDT because the photosensitizing drug makes your skin and eyes very sensitive to light. This is called photosensitivity. It usually lasts 4 to 12 weeks after treatment, but it can last longer. Your healthcare team will give you instructions on how to protect your eyes and skin after PDT.
Electrocoagulation or argon plasma coagulation
Electrocoagulation uses an electrical current to destroy cancer cells. Argon plasma coagulation uses argon gas and a high-frequency electrical current to destroy cancer cells.
Electrocoagulation or argon plasma coagulation may be used to treat Barrett's esophagus. They may also be used to treat symptoms of advanced esophageal cancer, such as difficulty swallowing.
These treatments may not be available in all Canadian treatment centres. Talk to your healthcare team to see if electrocoagulation or argon plasma coagulation is a treatment option available to you.
Esophageal dilation
An esophageal tumour can grow and block the esophagus so that you can't swallow. Esophageal dilation is a procedure that opens up an area of narrowing, or stricture, in the esophagus caused by the tumour.
The doctor uses an endoscope to put a tube called a dilator down the throat to stretch the narrowed part of the esophagus. Some types of dilators are flexible tubes. The doctor can use a series of bigger and bigger tubes to open the esophagus. Other types of dilators use a balloon to open the esophagus.
You may have esophageal dilation several times over several weeks to effectively open the area. In some cases, dilation is only temporary because the blockage can come back.
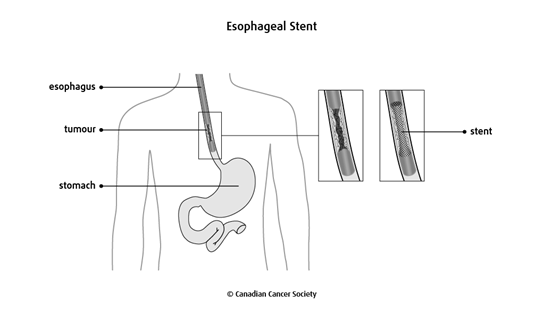
Esophageal stent
A stent is a metal or plastic tube that is placed in the esophagus to help keep it open. Some stents are made of a flexible mesh so that they can expand inside the esophagus.
Stents stop a tumour from completely blocking the esophagus. A stent can also be used to open up a narrowing (stricture) of the esophagus or to close abnormal openings (fistulas) between the trachea (windpipe) and the esophagus.
If the esophagus is blocked by the tumour, you may need to have esophageal dilation so that there is an opening for the stent. The stent is placed using an endoscope passed through the mouth and into the esophagus. After the doctor places the stent, an x-ray is taken to make sure it is in the proper position.
A stent allows you to swallow, but you will need to follow a special diet to help make sure that food doesn't get stuck in the stent. To reduce this risk, make sure that you:
chew your food thoroughly
avoid fibrous food, such as beef and chicken
drink carbonated beverages with your meals
The main risks of esophageal stents are the tumour growing into the stent, food blocking the stent or the stent moving out of position so that it needs to be replaced or removed.
Placement of a feeding tube
Feeding tubes are used to give you liquid nutrition to help you maintain your weight. Medicines may also be given through a feeding tube.
You may need a feeding tube before or after surgery. A feeding tube may also be used if a tumour causes a blockage that can't be removed or bypassed.
A percutaneous endoscopic gastrostomy (PEG) tube is placed during surgery for esophageal cancer. If no surgery is planned, then a feeding tube may be placed using an endoscope. The doctor passes an endoscope through the mouth, down the throat and into the stomach. The doctor then uses the endoscope to help guide the placement of the feeding tube.
A nasogastric feeding tube is a long, thin, flexible tube that is inserted through a nostril, down the esophagus and into the stomach. Once the tube is in the correct place, the end of the tube is taped to your nose or cheek to keep it in place. Nasogastric tubes are usually used if nutritional support is needed for less than 6 weeks.
Find out more about tube feeding.
Side effects
Side effects can happen with any type of endoscopic treatment for esophageal cancer, but everyone's experience is different. Some people may have many side effects. Other people have few or none at all.
Endoscopic treatments don't usually cause many side effects, but there can be problems or complications due to the treatment. These may include:
- bleeding
- narrowing (stricture) of the esophagus
- a hole (perforation) in the wall of the esophagus
- pain in the chest or abdomen
- an abnormal opening between the esophagus and windpipe (fistula)
